Investigating acquired resistance to G12C inhibitors in KRAS G12C mutant non-small-cell lung cancer
Meet Dr George Morrissey, a Clinical Research Training Fellow (CRTF) funded by the Cancer Research UK Manchester Centre supervised by Professor Angeliki Malliri, who began his PhD in 2020 and is due to finish in August 2024. His work is focused on combating resistance to KRAS inhibitors in lung cancer.
Lung cancer is the leading cause of cancer death worldwide, causing 35,000 deaths in the UK each year. As a result, it’s one of CRUK’s four cancers of unmet need.
Around one in four lung cancer patients have a mutation in a gene called KRAS, which is often associated with a history of smoking. Researchers at the MCRC are striving to better understand how these lung cancers progress, hoping to identify better treatment options and improve prognoses.
We speak with George about his journey into cancer research, being a clinical researcher at MCRC, and what his typical week looks like.
“It’s all very good and well, finding mechanisms in the laboratory. But what’s really important is whether this is what happens in patients in real life. And if it does, what can we do about it?”
~ Dr George Morrissey
CRUK Manchester Centre Clinical Research Training Fellow

What does your research involve?
Our understanding and treatment of lung cancer has been massively improved by identifying specific mutations that cause the disease to progress, known as driver genes. Through the use of inhibitor drugs, we can now block specific signalling pathways which are switched on in cancer cells and not switched on in ‘normal cells’. This enables you to treat the cancer with fewer side effects than we normally see with treatments such as chemotherapy, which has been the backbone of anti-cancer therapies for over 50 years.
In about 40% of lung cancer cases, we can identify a mutation where a drug can be used to stop that increased signalling. However, a current roadblock is that these drugs only work for about 12 months before the cancer starts growing again.
In my Clinical Research Training Fellowship, I’m looking at patients with tumours that have a mutation in a gene called ‘KRAS’. This is a driver gene which tends to be mutated in tumours from patients with a significant smoking background, and who often have other health problems. By culturing these cancer cells in the laboratory with the inhibitors, the aim is to try and understand how cancer driven by the KRAS gene becomes resistant to this newer type of therapy.
Currently, we’re collaborating with teams from The Christie to get hold of primary samples from patients who are about to start these therapies to see if what we’re seeing in the laboratory is the same as what we’re seeing in the clinic.
What inspired you to go into cancer research?
Between my foundation and intermediate training as a doctor, I spent a year working as a research fellow with the 100,000 Genomes Project at St. George’s in London, which piqued my interest in cancer genomics.
During my core medical training I had an oncology job at Charing Cross, which I really enjoyed. It was around this time that I was fortunate enough to attend the National Cancer Research Institute meeting in Glasgow, which drew my attention to some of the research that Manchester Cancer Research Centre has been a part of.
I’m originally from the North-West so I knew of The Christie already; its strong local reputation means it's quite exciting to be able to work here.
Dr George Morrissey
What does your typical work week look like?
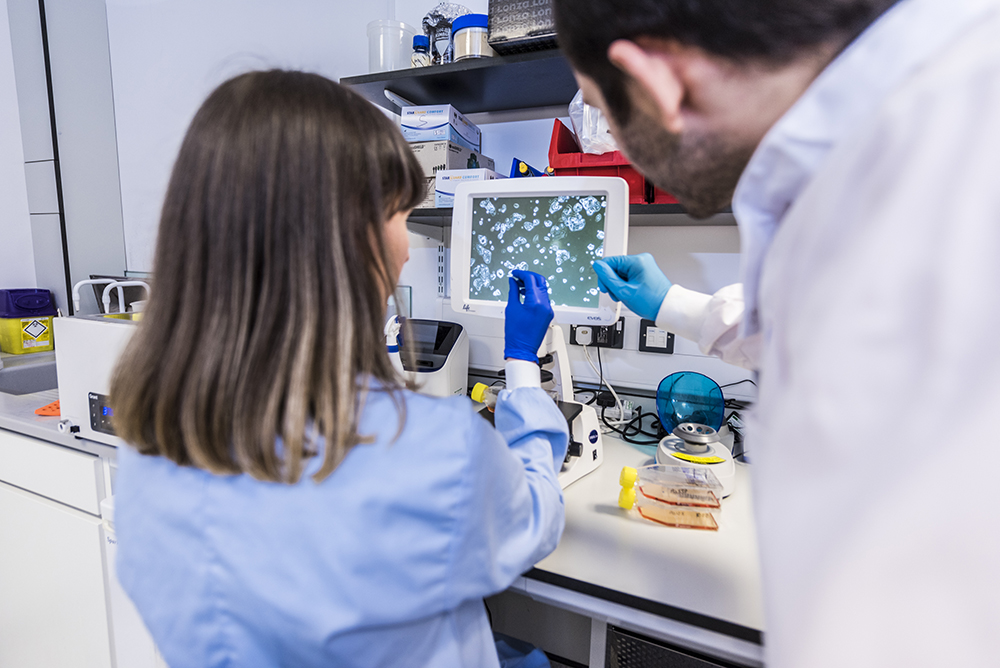
Monday is a busy day of tissue culture. This is a bit like being a gardener; you go in look at your cells and review whether they are ready to seed out experiments with. This would involve taking different populations of cells, treating them with different drugs, and then reviewing them later in the week.
On Tuesday, I tend to do a lot of western blots, which is how we look for changes in protein expression across different experimental conditions to try and infer differences in cell signalling.
One of the best things about being in Manchester is we have fantastic external speakers come in every Tuesday. I make every effort to go to these guest lectures, whether it is about lung cancer or not. I love being a clinician and especially being a bit older, you really appreciate having time in your day to go away and learn something. On Wednesday, I’ll do my best to catch up with any new papers that I have caught sight of over the last week or so. We also have lab meetings every Wednesday afternoon, where every month I’ll update the lab about my progress in my project.
On Thursdays, I usually have a meeting with clinicians and scientific officers at The Christie, focused on translational aspects of the research such as recruiting patients with KRAS mutations to take part in longitudinal, observational studies. Thursday will also be another busy day of tissue culture.
On Friday mornings I will usually do my analysis for the week before heading into the clinic in the afternoon to consult with patients.
We need to view resistance differently. There's increasing evidence from my work to show that resistance emerges as a process- rather than as a predetermined inevitability. What we tend to do clinically is a biopsy before treatment, and a biopsy at resistance. What we don't do is ask: ‘what's happening in the middle?’ How do we get from A to B?
Dr George Morrissey
What’s the best part of your research?
I really enjoy the clinical side of it because you’re seeing patients who are on the drug that you are investigating, which helps the science feel more real. Clinically, at the end of each day, you feel like you might have achieved something, even if it’s only just prescribing a medication or exploring a patient’s concerns. This gives balance to laboratory research, where you might spend months designing and optimising an experiment which might not work.
What is the most challenging aspect of your research?
I think the hardest part of doing a clinical fellowship is that you have to be good at both the science and being a clinician. So effectively, it’s like having two jobs at once. And yes, that’s tricky, but it’s also very rewarding. I’m as much of a scientist as everyone else in the lab, but I’m a doctor as well. And I think that’s the hard thing: you have to master both sets of skills, rather than just focusing on one.
What advice would you give to someone thinking of applying for a Clinical Research Training Fellowship?
The biggest thing I wish I had known was the different pace; things in the lab take longer than you’re used to in the clinic. Equally, it’s important to remember to be kind to yourself. You’re here to train and learn, so don’t get disheartened if after the first six months you think ‘gosh, I’ve not really changed anything’. You will have learned lots of different things that you haven’t even begun to appreciate. What I’m most proud of is when I look at what I can do now compared to what I could in the beginning; I’m like a totally different person.
Useful resources
Cancer Research UK lung cancer resources and support organisations
This article was written by MSc Science Communication Student Emily Stephenson as part of a project placement at Manchester Cancer Research Centre.
Clinical Phd Studentships
Discover more information about the postgraduate clinical research programmes available in Manchester.
Research Opportunities
Discover the research opportunities available to at the CRUK Manchester Centre
Researcher Stories
Read more stories from our researchers about their experiences of studying in Manchester
One in Two: A Manchester Cancer Research Podcast
The basic biology of lung cancer with Dr Colin Lindsay: Exploring oncogenic drivers such as the KRAS mutation.